Présentation
POI is a heterogeneous syndrome, often leading to infertility and associated comorbidities. Its prevalence is 1-4%, making it a public health concern. It is clinically defined by amenorrhea or spaniomenorrhea > 4 months, with an FSH level > 25 IU/L in women under 40 years of age.
There is considerable genetic heterogeneity associated with this syndrome. Karyotyping rules out Turner syndrome or chromosomal rearrangements. Molecular biology testing rules out FMR1 premutation. Targeted high-throughput sequencing (panel) can rule out a pathogenic variant in known candidate genes. To date, more than 130 genes responsible for POI have been identified.
Rare oocyte abnormalities include oocyte maturation defects (OZEMA: Oocyte, Zygote, Embryo Maturation Arrest) and oocyte dysmorphies. To date, more than 30 genes have been implicated in the occurrence of this phenotype.
The subpopulation eligible for genome sequencing corresponds to patients with undiagnosed conditions. Accurate genetic diagnosis will enable appropriate genetic counseling based on the cause (patient and family), the implementation of monitoring to detect possible comorbidities, and appropriate prevention and treatment.
Criteria before considering a discussion in MDM-FMG
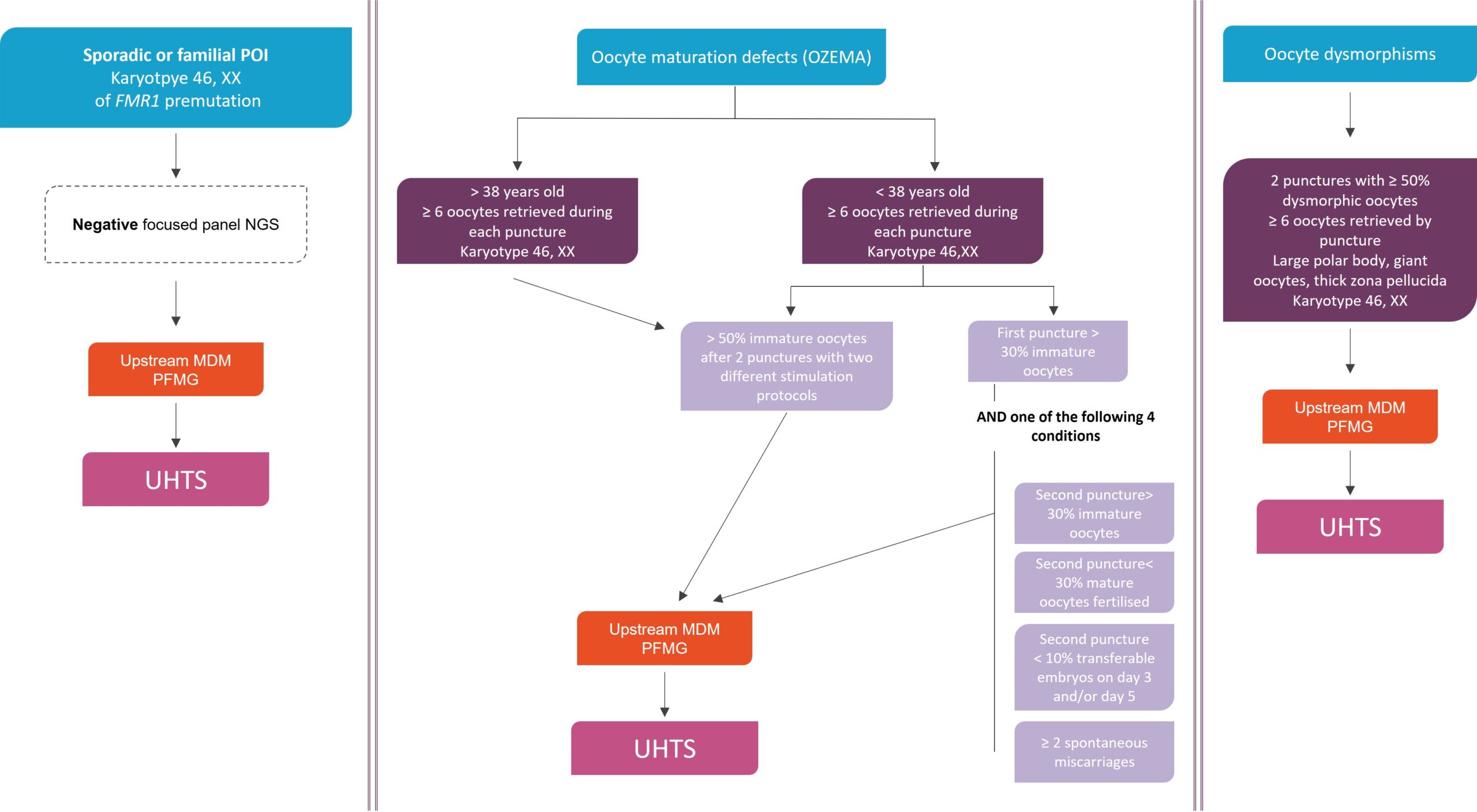
1°) POI
Clinical:
- POI = amenorrhea or spaniomenorrhea > 4 months in women under 40 with FSH > 25 IU/L
- Specify whether familial or sporadic.
- Rule out some etiologies of POI ( chemotherapy, radiotherapy, surgery)
- Search for clinical or biological autoimmunity (patient, family)
- FSH, LH, E2, AMH
- TSH, antithyroid antibodies and anti-adrenal antibodies (anti-21-hydroxylase)
- Ovarian ultrasound to evaluate the ovarian size and the presence of follicles
Genetics:
- Normal karyotype
- Negative FMR1 premutation testing
- Negative targeted NGS panel (note date, number of analyzed genes, geneticist)
- Prior consent of parents (for trio) strongly recommended
2°) Rare oocyte abnormalities:
- Women with primary (or secondary) infertility of idiopathic origin
- Pedigree, specifying any history of miscarriage
- Favorable response to ovarian stimulation, ≥ 6 oocytes collected
- 46,XX caryotype
Prior consent of parents (for trio) strongly recommended
UHTS in diagnostic strategy
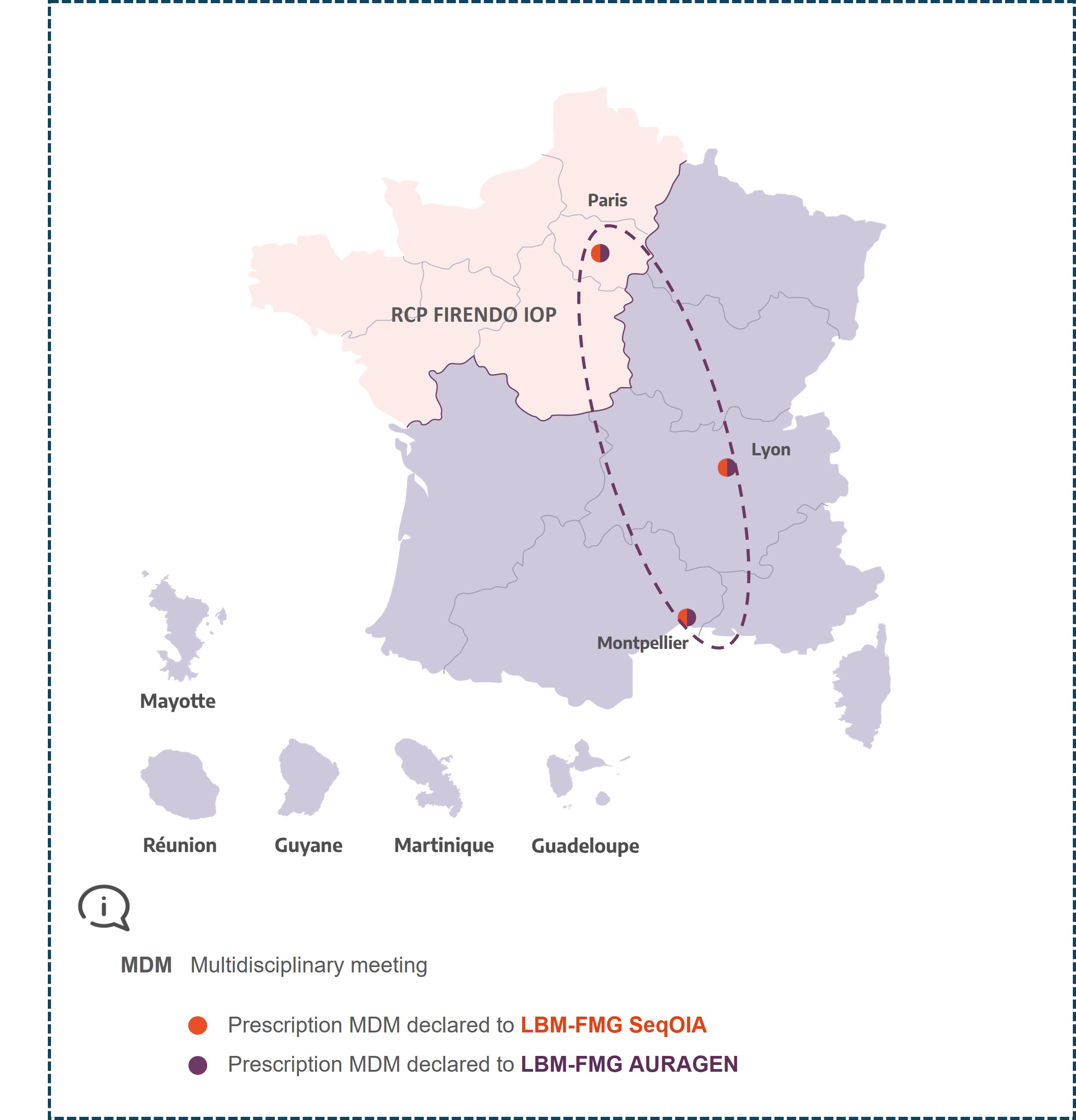
MDM FIRENDO IOP
Paris
Sophie Christin-Maître
sophie.christin-maitre@aphp.fr
Michel Polak
Montpellier
Françoise Paris
Lyon
Laetitia Martinerie
laetitia.martinerie@chu-lyon.fr
Aude Brac de la Perriere